Best COPD Inhalers Inhalers are designed to deliver medication directly to the lungs, helping to open airways, reduce inflammation and make it easier to breathe. Zemaira is an injectable medication that helps people with alpha-1 antitrypsin deficiency (a genetic condition that can worsen COPD). 1. Zemaira (α1-proteinase inhibitor) By increasing levels of the α1-proteinase inhibitor in the body, Zemaira helps protect the lungs from further damage. It's not a traditional inhaler, but it is an important treatment for people with specific COPD-related conditions. 2. Spiriva (tiotropium) Spiriva is one of the most commonly prescribed inhalers for people with COPD. It helps relax and open up the airways, making it easier to breathe. It is a long-acting bronchodilator, meaning it works for up to 24 hours, providing day-long relief. This inhaler is typically used once a day. [youmaylike] 3. Advair (fluticasone/salmeterol) Advair is a combination inhaler that contains both a steroid and a long-acting bronchodilator. The steroid works to reduce swelling and inflammation in the airways, while the bronchodilator helps relax the muscles around the airways. This combination helps improve breathing and prevent flare-ups of COPD symptoms. It’s typically used twice a day. 4. Symbicort (budesonide/formoterol) Like Advair, Symbicort is another combination inhaler with a steroid and a bronchodilator. It helps reduce inflammation in the lungs and opens the airways. This inhaler is also used to treat asthma, but it’s a great option for managing COPD as well. It is taken twice a day for the best results. 5. Breo Ellipta (fluticasone/vilanterol) Breo Ellipta is a once-a-day inhaler that combines a steroid and a long-acting bronchodilator. It helps open the airways and reduces inflammation in the lungs. This inhaler is typically used for people with chronic COPD symptoms to help improve lung function. 6. Albuterol (ProAir, Ventolin, Proventil) Albuterol is a short-acting bronchodilator that provides fast relief for sudden breathing problems, like shortness of breath or wheezing. It works quickly to open the airways, helping you breathe easier. It is often used as a rescue inhaler during flare-ups and should be kept on hand for emergencies. 7. Atrovent (ipratropium) Atrovent is another short-acting bronchodilator. It helps relax the muscles around the airways and can be used in combination with other medications to treat COPD. Atrovent is often used multiple times a day and can help reduce coughing and wheezing. COPD Control and Relief There are many inhalers available to help manage COPD symptoms, but the best one for you depends on your specific condition and treatment needs. Zemaira is an important option for people with alpha-1 antitrypsin deficiency, while other inhalers like Spiriva and Symbicort help open the airways and reduce inflammation. Speak with your doctor to find the right inhaler for you, and remember that proper use of your inhaler is key to managing your COPD and improving your quality of life. Read on to learn about exercise induced asthma, and how you can cope with it.
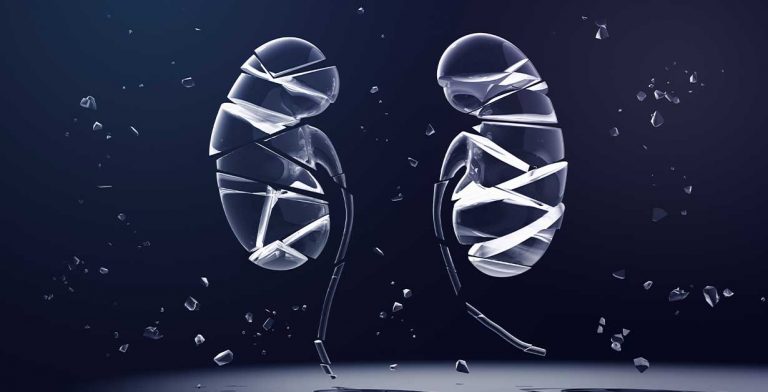
Stage 3 Kidney Disease Explained
In this article we look at the most common symptoms of kidney disease. If you've ever wondered, “what is stage 3 kidney disease?" then you are in the right place.
Do you think you or someone you know might have it? This article will explain what kidney disease is, the causes and symptoms, and we will go over how someone can get a proper diagnosis and begin treatment.
Symptoms of Kidney Disease
The early stages of kidney disease may not have any noticeable signs or symptoms. However, as kidney disease progresses, more symptoms are evident. Usually, when symptoms of kidney disease appear, there is a significant loss of kidney function.
Some of the symptoms are nonspecific or can be a result of other diseases, but other risk factors can lead to a suspicion of kidney disease. Symptoms of late stage kidney disease may include:
- Headaches
- Loss of appetite
- Nausea or vomiting
- Weight loss
- Itching or numbness of the skin
- Fatigue, or feeling tired most of the time
- Changes in behavior or sensorium
- Chest pain
- Shortness of breath
- Pallor or anemia (low hemoglobin count)
- Decreased amount of urination
- Sleep problems
- Swelling of extremities or generalized swelling
Understanding Kidney Disease
Put simply, kidney disease occurs when there is damage to the kidneys. The kidneys are bean-shaped organs that are responsible for the filtration of blood and remove waste through the production and excretion of urine.
Kidney disease can be acute or chronic. Acute kidney disease usually lasts days or weeks, while chronic disease lasts months to years. As a person gets older, the chances of getting kidney disease increases, especially if that person has any risk factors, which may include:
- Comorbidities such as hypertension, diabetes, or cardiovascular disease
- Smoking
- Obesity
- Family history of kidney disease
- Congenital disorders or abnormal structure of the kidney
- Old age
It is important to detect kidney disease early so that appropriate treatment can begin. This will help prevent permanent damage to your kidneys and help avoid life-changing treatment, such as dialysis.
What Causes Kidney Disease?
There are many different causes of kidney disease. Some are genetic, while others are acquired or due to a person’s environment and lifestyle.
The most common causes of kidney disease include diabetes and high blood pressure. Diabetes causes kidney disease by damaging the filters of the kidney, which leads to the leaking of important substances, such as a protein that is needed by the body.
Hypertension causes kidney disease by damaging the blood vessels of the kidney. These injuries make the kidney do a poor job of filtering wastes and in severe cases leads to the buildup of harmful toxins in the body.
Other causes of kidney disease may be infections, toxins, drugs, or congenital or autoimmune diseases. Examples of other causes of kidney disease may include:
- Autoimmune diseases, such as Goodpasture’s disease or nephritis from lupus
- Genetic conditions, such as Alport syndrome or polycystic kidney disease
- Infections and their complications, such as pyelonephritis or glomerulonephritis
- Drugs or toxins, such as lead poisoning
- Renal artery stenosis
Stages of Kidney Disease
Chronic kidney disease is when there is an irreversible injury to the kidneys over a long period. It has five different stages which represent the condition and function of the kidney.
Stage 1 kidney disease occurs when the disease has just begun, and stage 5 indicates complete kidney failure. As the disease progresses, your kidneys have a harder time filtering your blood, and if it progresses to stage 5, they stop functioning altogether.
According to the American Kidney Fund, stage 3 kidney disease occurs when a patient’s estimated glomerular filtration rate (eGFR) is between 30 and 59. There is moderate kidney damage, but they are still able to function.
Symptoms do not usually show in stage 3 kidney disease. However, if you experience any swelling in the hands or feet, back pain, or frequent urination, it could be an indication. Don’t hesitate to make an appointment with your doctor if you feel like something is off.
Stage 3 Kidney Disease Diagnosis
During stage 3, the damage to the kidneys is moderate and the loss of kidney function is evident. As mentioned above, a patient’s eGFR values are found to be in the range of 30 to 59.
Other laboratory examinations can be used to determine kidney disease as well. These include checking a protein called albumin in your urine, which is not usually present in patients with normal kidneys. Albumin is normally filtered and stays in the blood, but in patients with kidney disease, due to the damage to the kidneys, it leaks out. Checking the albumin not only helps determine if kidney disease is present, but also evaluates response to treatment.
A patient’s kidneys can also be evaluated through imaging, especially if the cause may be genetic.
Is it the end of the world if you are diagnosed with stage 3 kidney disease? Despite having a noticeable change in kidney function, there are still things that can be done.
The goal for patients with this stage of kidney disease is to avoid further progression. Kidney disease will worsen over time if nothing is done to prevent its progression. This is important because kidney damage can be permanent.
Treatment Options for Kidney Disease
It is important to identify kidney disease because early detection can prevent progression to irreversible kidney damage. Stage 3 kidney disease can usually be cured without dialysis or a kidney transplant.
There are medical and non-medical options for kidney disease, but the goals of therapy are to treat the underlying cause and to prevent further progression of kidney disease. Medications to control hypertension and diabetes are wide and varied. Other medications to treat other causes of kidney disease are also available (for example, antibiotics for infection).
Further medications can be given for complications of kidney disease (iron supplements for patients with anemia, calcium supplements, and medications to induce urination for those with decreased urine). A consult with a nephrologist who specializes in kidney disease is also important.
Non-medical options include changing diet and lifestyle. These include decreasing salty food intake, increasing physical activity, stopping smoking, and stay within the ideal body weight. These changes are important for patients with Stage 3 kidney disease because they will help halt progression.